by Adam Grybowski
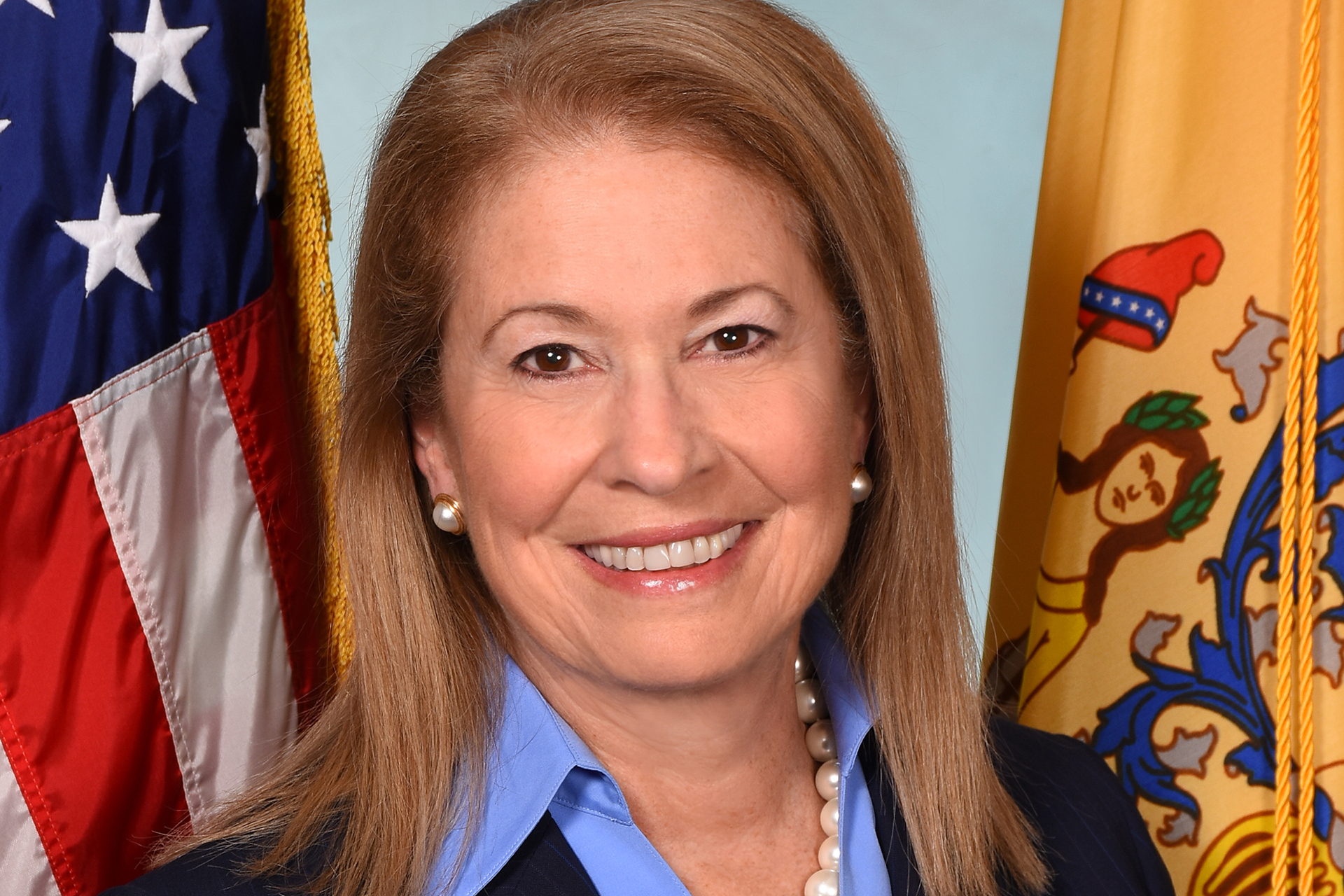
After serving as acting commissioner of health for about six months, Judith M. Persichilli '80 was confirmed by the State Senate on Jan. 9, 2020, to become New Jersey's new health commissioner. At the time, a novel virus first identified in Wuhan, China, was just beginning to make its way around the globe. Only three months into her tenure, the World Health Organization officially declared a pandemic underway, upending daily life and significantly raising the stakes for health officials like Persichilli.
In this interview, conducted in October, Persichilli, a former Rider Trustee who received a Master of Arts in the University's Program for Administrators, reflects on her experience leading the state through a once-in-a-lifetime public health crisis.
When you were confirmed in January, what did you think your top priority would be as you officially began in the role?
When I accepted the position as acting commissioner a little over a year ago, I did it because I thought I could contribute to the state where I was born and where I’ve lived my entire life.
I knew it would be a challenge because of the many health issues that confront us as a state. But after only five months on the job, we started to get reports of a novel virus in Wuhan, China, and what has followed with more than 14,676 confirmed deaths and more than 263,495 cases in New Jersey is similar in some ways to the 1918 Spanish flu pandemic that killed my grandmother at the age of 36.
COVID-19 has confronted all of us with the challenge of a lifetime and has impacted every aspect of our lives — how we work, how we interact with family and friends, how we go about everyday living, how we go to school or travel, and more.
How has your background as a nurse and hospital executive influenced your approach to fighting the coronavirus in New Jersey?
Throughout my career, I’ve always believed that frontline workers are vital to making the necessary changes to promote better health in our communities because they have both the knowledge and experience.
One of the values I’ve found most important, first working as a nurse in a fast-paced ICU and then as a nurse educator before moving into health administration, is having a strong team by your side.
My first 14 months at the Department have been filled with long days and hard work, but the Department of Health team has been incredible. The staff of the Department rose to the occasion, working tirelessly — including weekends through February, March, April and May — as did our health care workers, first responders and certified nursing assistants in long-term care facilities.
This once-in-a-century pandemic requires an all-hands-on-deck response. The team at the Department, all seasoned public health professionals, worked around the clock to ensure the safety of the residents of New Jersey. My experiences in leadership taught me to trust them; to give them a seat at the table; a voice in decision making and the chance to make a difference and, in reality, to be part of making history. They did not disappoint. The more I asked, the more they gave. All of them taking on tasks they had never done before — setting up field medical stations and isolation beds in closed hotels; developing testing sites; monitoring international supply chain disruptions; building our own strategic stockpile and the list goes on. I directed the orchestra toward a common goal, and they performed expertly.
What has been the single biggest challenge facing New Jersey as officials seek to contain the virus?
We faced not only a medical challenge but the disruption of international supply chains of Personal Protective Equipment (PPE) and life-saving equipment like ventilators, hospital bed capacity concerns, and being able to care for our most vulnerable and fragile residents.
In expectation of the predicted surge, hospitals doubled their critical care capacity and the
Department worked with the federal government to set up field medical stations and open closed hospitals and wings to provide additional bed space.
As part of the response, the state also undertook an unrelenting search for PPE and ventilators, from the White House Strategic National Stockpile to third-party vendors. Now that the second wave is upon us, the state is continuing to build its stockpile of supplies.
Our long-term care facilities have also been at the epicenter of the pandemic. Although the number of outbreaks in these facilities has decreased, there are still more than 165 active outbreaks. So, we are still very concerned about the vulnerable residents of these facilities.
Gov. Murphy’s budget invests more than $1 million to boost the resiliency of these facilities by creating an Office of Long-Term Care dedicated to assisting these facilities in improving their infection control measures, among other things. The Department has implemented more than two dozen of the reforms recommended in a report by an independent consultant to strengthen the resiliency of these facilities and improve the quality of care. The Department has also issued detailed guidance on reopening that requires facilities to meet certain benchmarks including adequate infection control, testing, staff and PPE.
In the U.S., the coronavirus has taken a disproportionate toll on the most vulnerable, including people of color and low-income Americans. Has that been true in New Jersey?
The pandemic has financially devastated families across our state, but especially those who were already vulnerable. Communities of color, many in our urban cities like Trenton, have been disproportionately impacted by the virus.
The same long-standing inequities that have contributed to health disparities affecting racial and ethnic groups have also put them at increased risk for COVID-19. These racial and ethnic populations are also disproportionately represented among essential workers and those unable to work from home as employees of places such as health care facilities, factories, farms and grocery stores.
Although Black residents comprise 13% of New Jersey’s population, they represent nearly one-fifth of the state’s lab-reported COVID-19 deaths. And Hispanics are more likely to die younger as a result of COVID-19 than their white and Asian counterparts. Forty-seven percent of deaths among those aged 20 to 34 were Hispanic.
How can those inequalities be addressed from a public health perspective?
For populations whose vulnerabilities are heightened by COVID-19 and for those who are newly vulnerable to the virus, we have used a health equity lens in all parts of the response and recovery. As we plan for a large-scale vaccination program, equitable access is a primary consideration across all planning and delivery elements.
Has your understanding of the virus changed in any significant way?
We’ve learned a tremendous amount since the beginning of this pandemic, which has informed our decision making moving forward.
Early on, it was thought we saw the most extreme impact on older residents, but as we grew to know, it affects people of all ages, including young adults, who, despite maybe feeling invincible, account for larger numbers of positive cases around the country.
People could be asymptomatic and still have the virus, and unknowingly spread it to others in the community.
We’ve also learned a lot about therapeutics and treatments to provide remedies for patients with COVID-19. As we await a safe and effective vaccine, some medical treatments, like Remdesivir, an antiviral drug, have been found to shorten hospital stays. Additionally, the steroid dexamethasone has been shown to reduce deaths of patients on ventilators by one-third.
But, what we know for sure is that the best course of action is to prevent getting sick in the first place by taking steps to protect yourselves and others by continuing to practice social distancing; wear a face covering; wash hands frequently for at least 20 seconds; and use hand sanitizer with at least 60% alcohol.
This once-in-a-century pandemic requires an all-hands-on-deck response.
How has the coronavirus affected your perception of New Jersey's health system in general?
I believe that we’ve all, myself included, learned important lessons throughout this pandemic. We know that we must strengthen our public health infrastructure — the workforce, information systems and agencies focused on community rather than individual health — to improve our ability to respond nimbly to COVID-19 and future pandemics.
How is New Jersey preparing for a COVID-19 vaccine, if and when one proves to be safe and effective?
The Department submitted a COVID-19 Vaccination Plan to the Centers for Disease Control and Prevention on Oct. 16 based on the work of our Vaccine Task Force. We formed nine workgroups tackling various aspects of establishing a large-scale vaccination program including public confidence, policy, logistics, special populations, IT, and management and administration. We also have a Professional Advisory and Health Equity Committee advising the Department on priority groups for vaccination.
What steps need to be taken for the state to be prepared for another pandemic?
A second wave of COVID-19 is now upon us and we are preparing based on lessons learned from our prior experiences. If individuals do not adhere to the social distancing and masking guidelines — the wave has the potential to become a surge. We have stockpiled PPE, the anti-viral Remdesivir and ventilators.
Our biggest concern will be staffing if individuals fall ill like in the prior surge. We know that this virus did not take a break. We also know that asymptomatic spread is more prevalent than initially thought so non-pharmaceutical interventions are even more important.
As the cold weather sets in and people move indoors — the threat of spread is even greater. We also know that we will be fighting this enemy for a longer period of time and hope that community protection through effective vaccination against COVID-19 takes hold.
To complement traditional contact tracing efforts, the Department launched a COVID ALERT NJ app for mobile devices, which Rider University has shared. It notifies users if they have been in close contact with someone who has tested positive for COVID-19. Knowing about a potential exposure can help individuals quickly make a plan to stay safe, including contacting their physician or the campus health center to get more information about quarantining and testing to prevent community spread.
Many continue to look forward to “going back to normal.” Is there such a thing?
As I mentioned earlier, the way of life we once knew has changed drastically to ensure that we contain the spread of COVID-19 in our state. And while we continue the road back to recovery, we must remain vigilant in reiterating precautions and practices that helped us to flatten the curve. We must adjust to a “new normal” going forward.
One of the values I’ve found most important...is having a strong team by your side.
Crisis communicator
Commissioner Persichilli isn't the only Rider graduate helping to lead New Jersey's response to the pandemic. Donna M. Leusner '80, the director of communications at the state Department of Health, received a Bachelor of Arts in Journalism from Rider and was editor of the University's student newspaper, The Rider News, as an undergraduate. Leusner was a reporter at The Star-Ledger for 21 years before joining the Department. This interview was conducted in October.
How important is it to communicate a clear, consistent message during a public health crisis?
Clear, consistent messaging delivered by trusted public health professionals can save lives. There’s a reason why Dr. Anthony Fauci is considered the nation’s most credible voice on COVID-19. He explains the virus, its treatments, vaccine trials and the importance of wearing a mask in simple terms we all understand. As a scientist at the National Institute of Health, physician and public health advocate, he has earned our trust for over 50 years.
Public health experts provide science-based information and resources and that makes it more likely that people will listen to their guidance. Physicians and nurses have strong, trusted relationships with their patients so it is important that health care professionals have the facts about the process leading up to the approval of a vaccine(s) so they can help us build public confidence in a vaccine. According to an Axios-Ipsos survey in late September, 62% of 1,000 adults surveyed said they would trust an endorsement of a vaccine if it came from their personal doctor. And that’s important because skepticism about a COVID-19 vaccine is very high — especially in a state like New Jersey, which has a very vocal anti-vaccine movement.
What effect has the decline of local media had on your role as a communications director?
I was a reporter for The Star-Ledger for 21 years. We had all day to write a 25-inch story and work with the graphics team and photo desk. Now, the news cycle is continuous and print stories are also online, posted on social media and are often accompanied by videos. There may be fewer newspapers, but there are many more digital outlets and cable TV stations reporting the news 24/7.
Is there a silver bullet to battling misinformation during a public health crisis?
The key is to provide timely and factual, science-based information to counter misinformation. And don’t repeat the misinformation that you are trying to counter. You may have to respond repeatedly as the situation changes. Educational materials/infographics/fact sheets must be updated and disseminated quickly through established channels including the Department website, sister state agencies and various professional organizations and community stakeholders.
The New Jersey Department of Health uses three social media platforms with a total of 100,000 followers to rapidly push out relevant information and to dispel myths, misinformation and misreporting of scientific evidence as it pertains to COVID-19.